FAQ Episode 76: What common element promotes PMS and provokes migraines?
Frequently Asked Questions about Natural Migraine Relief
If you are still pre-menopausal, there is a pretty high chance that you have some degree of premenstrual syndrome (PMS). Some 70-80% of women have some version, which includes a wide range of recurrent symptoms that occur anywhere from several days to two weeks before your period. From among this group, around 20-40% have significant complications, including migraines, as a secondary result.
Common symptoms of PMS
fluid retention and related weight gain fluctuations.
breast fullness or tenderness.
abdominal bloating, feeling ‘gassy’ and a sense of ‘irritable bowel’ which can include cramping as well as constipation and/or diarrhea.
headaches, especially migraines.
generalized muscle aches or cramps.
fatigue, lower stamina through your day.
oily skin or acne breakouts.
feeling irritable, with a reduced tolerence for other people’s drama.
appetite changes, especially cravings for carbs, salt or alcohol.
cognitive problems including focusing and memory recall.
depression with feelings of sadness, social withdrawal.
anxiety or tension, with irritable or even hostile behaviour.
changes in sex drive, most often a decline.
insomnia.
Many women with PMS have ‘learned to live with it’, especially if they have dealt with since their teen years. With situations like this, trying to figure out what’s normal is like asking a fish what it means to be wet. I’ve found that keeping a calendar of both menses and symptoms over 1-2 cycles allows you to ‘see the forest for the trees’. See the Women’s Assessment Calendar1 that I ‘ve used for my patients over the last 35 years. This includes details on its use and a printable version at the end of this post.
The role of estrogen dominance in PMS and migraine
Despite the broad range of potential PMS symptoms, there is one key hormonal imbalance that can provoke most all of them, and that is estrogen dominance. This doesn’t just mean excess estrogen, but rather having too much estrogen for the amount of counter-balancing progesterone. If you don’t produce enough progesterone in the latter half of the month, even a modest amount of estrogen can be problematic. A common example of this would be for women who are in perimenopause, where ovarian output is steadily dropping oven a time frame that usual covers many years. These individuals can be both estrogen deficient (meaning the absolute amount, compared to previous years) while also being estrogen dominant (which is a relative ratio, because the comparable progesterone levels are even proportianately lower). Some individuals, even those with regular menses, have underproduced progesterone for years, maybe even dating back to the onset of puberty. Does every set of ovaries know exactly what to do right from the start, and do it right, every single month?. What if they missed the lectures about optimal progesterone production back in their “Intro to Puberty” class? If this is to any degree your story, you should read on, as the next portion of this post can be life changing.
The role of progesterone in brain health
The pharmaceutical industry has multiple agents that can act specifically on symptom suppression for PMS, such as:
diuretics for fluid retention
psychotrophic and antidepresseant meds for anxiety and depression
estrogen suppression meds to minimize estrogen dominance symptoms
inhibitors for excess uterine prostoglandin production leading into menses
cycled hormones (oral contraceptives) to manipulate the menstrual cycle and ovulation
There are also multiple pharmaceuticals aimed at either preventing or minimizing migraine events or managing the associated pain. I’ve no doubt that the readers of this post, as a group, have tried most of them at one time or another.
While all of these may have their place; as in many interventions in medicine and in life, it makes sense to start with the simplest and safest therapy that covers the most potential bases. That would be targeted bio-identical progesterone support therapy.
Progesterone is amazingly safe to use. You can actually buy it over the counter. When the FDA allows you to walk out the store with 25 jars of “Progesterone USP”, you know the safety index has to be rather high. That doesn’t mean that that overuse might not have potential side effects. I’ve listed some concerns related to overuse or misuse in the footnotes.2
Let’s talk first about whys for progesterone therapy, and then the details about the how.
The why for progesterone therapy
Progesterone has multiple receptors and functions in every cell type in the brain. Optimal levels can influence the expression of both PMS and migraine. Keep in mind here that we are looking at bioidentical progesterone, NOT the synthetic progestin family emphasized by the pharmaceutical industry.
Appropriate, and when indicated, augmented levels of progesterone can:
increase the production of GABA, a neurotransmitter that promotes sleep and also enhances mood by inducing feelings of relaxation and well-being.
provide a counterbalance to the side effect prone aspects of estrogen, especially when the latter has had an excess influence.
protect the brain from damage and promotes repair after injury. This is not only true for more serious cases like traumatic brain injury, but also the micro-trauma induced by repetitive migraine headaches.
promote myelination, neuroprotection, and temper neuropathic pain, like that experienced in migraine.
when taken orally can provide progesterone metabolites with sedative and even hypnotic effects that can augment sleep quality. A lack of brain repair during sleep can be a promoting factor for migraines. Topical progesterone doesn’t have these same downstream metabolites converted in the liver, so an oral dose can be more effective than topical in this regard.
can protect or rebuild the blood-brain barrier (BBB). The BBB both keeps toxins out, and supports healthy neurotransmitter levels within the central nervous system.
The how of progesterone therapy
For the purposes of this discussion, let’s stay with progesterone that you can buy over the counter, versus that from a compounding pharmacy. It should be labeled “USP”, that is to say, pure bioidentical progesterone, not “Wild Yam cream” or another plant precursor that cannot be quantified. Look for a brand that tells you the milligram amount of each dose right on the label.. Many versions provide 15 mg/gram, which is an useful dose with which to start. If it also comes in a pump container, that can be useful. Many pumps deliver 1.3 grams or ~22 mg progesterone per dose. Some brands will say “400 mg in 30 grams” which is only 13.3 mg/gram. To give you an example on price, the NOW brand Progesterone cream with pump dispenser delivers about 1.3 g of cream per pump providing 20 mg of USP Progesterone. This $13.50 product delivers 70 pumps, or 20 cents per 20 mg progesterone. Figure your daily cost from the recommendations below.
Let’s consider therapy for someone who has 1) PMS symptoms, of which 2) migraine headaches are more prominent, occuring in the latter third of the cycle. Using the Assessment calendar (see below) can help for you to better define the days needing support therapy. Next:
start with 15-30 mg of progesterone, applied at night, starting 1-2 days before the part of the cycle that is most symptom prone. For most, this would be ~5-10 days per cycle (or as per your calendar). Stop using the progesterone when you reach the last evening of your normal cycle duration. So, if you typically have a 28 day cycle, you would use the last PM dose on Day 27. For this example, if you start your menses around Day 28, that Day 27 application would be your last day of use for that cycle. If for some reason you start sooner than Day 28 (for this example), then the PM of that day would be your last application for that month’s cycle.
rotate the sites of application among your four extremities in turn. For instance, on four consecutive nights you might use 1) the right inner arm and/or bicep, then 2) the left inner arm and/or bicep, then 3) the left inner thigh and lastly 4) the right leg inner thigh. Then begin the cycle again. You will apply the cream to a patch of ~ 2-3” X 4-6” of skin. Use 2 fingertips to spread it thin, you don’t have to “rub it in.” It should absorb nicely over 8-12 minutes. Use in the hour before bedtime is the best time for brain and sleep benefit, although morning can be used if that better suits your schedule.
keep the Assessment Calendar to follow your progress. If you are doing better, but with more than 50% room for improvement, increase the dose by adding 15-20 mg/day, still in the PM, for the next cycle. You will need to use more skin, but the sites mentioned above should have plenty of room for even 2-3 grams of topical cream.
if your headaches are better during the time of progesterone application, but still present the other parts of the month, you may benefit from using some progesterone all month long, even on the days of menstual flow. In this case, you could start with 20 mg progesterone every day, and double that amount on the “PMS prone” days. Continue to keep the calendar to look for effectiveness and trends in symptoms, including headaches.
if you feel that you need additional help on individualized dosing, look for a local compounding pharmacy (Google “compounding pharmacies near me”) and talk with their compounding pharmacist about local healthcare resources who can more specifically individualize your hormone support therapy. I’ve found that some of my patients benefitted from progesterone doses that were much higher (100-400 mg topical or topical+oral per day), or that required dosing regimens that gave variable and phased support throughout their cycle. This can be complicated and may benefit from the oversight of an experienced clinician.
If you would like more detailed information on hormone support for migraines, take a look at this blog’s affiliated online course Natural Migraine Relief for Women, especially Lessons 11-14 which look at Female Hormones as root cause factor for women throughout the reporductive life cycle.
Keep in mind that hormone support as described above may be only one of several root cause factors that you need to identify and manage on the path to finding your version of migraine relief
Please also remember that this or any other Natural Migraine Relief post is not designed to replace your doctor or a thorough initial workup for your headaches, or to give you one-to-one medical advice.
You’ll get an email from me once or twice a week. Please subscribe for ideas to help you manage your migraines both naturally and effectively.
I’d appreciate it if you share this with friends, family or colleagues who may find value in reading this post.
Lastly, leave a like or comment as it helps others find Natural Migraine Relief on Substack! It only takes 2 seconds and helps me a bunch.
The Women’s Assessment Calendar
These 44 symptoms cover most PMS related symptoms. You can see the spaces left blank at the end for you to track any other self-defined symptoms you wish to write in. The numbers at the top are the calendar days of the month, while under “SS- Menses” near the bottom of the page you track the menstrual days of the cycle, using the simple legend there for menstrual activity (leave blank if none on any given day).
For any given day, use the Symptom Rating Scale to put a 1, 2, or 3 in the box for any applicable symptom. Leave the other boxes blank to keep it focused. Later, this can also help you see symptom clusters ‘jump out at you’ when look at the month as a whole. You may even leave off marking the “1s” for the mildest symptoms, to make it easier to see the more symptom prone #2’s and #3’s clusters within the cycle. Our goal in this exercise is:
to see what, if any, symptoms you’re experiencing. It’s easy 2-3 weeks later to have forgotten the details if you didn’t record them right at the time.
to see if these symptoms, especially headache, correlate with roughly the latter third of that month’s cycle (the luteal phase), which would indicate a probable progesterone deficit/estrogen dominance as a key contributing factor.
Side effects of excess progesterone
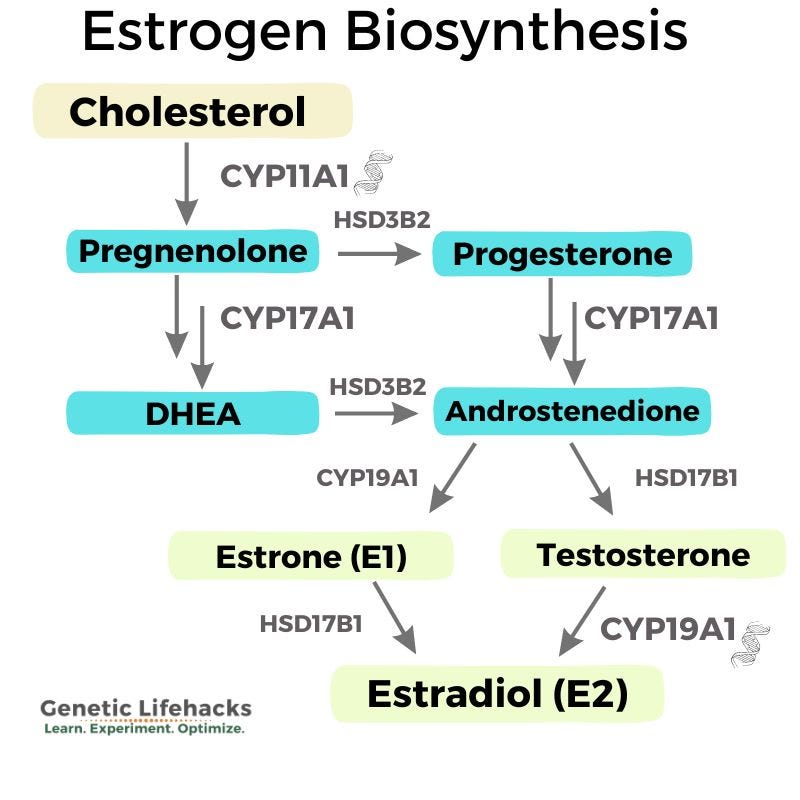
Excess amounts of progesterone can be made into side products, including testosterone and estrogen, as you can see in this schematic:
This potential side product excess could result in some of the symptoms we are seeking to alleviate, like headache, fluid retention or breast tenderness. Such hormonal overflow excesses over time could also pose concerns for those with an at-risk history for breast cancer, heart disease or clotting disorders. It could also affect both the ability to get pregnant or to carry a successful pregnancy.
At higher doses, progesterone can cause a sense of drowsiness (which could be fine at bedtime) but this should be considered when used during working hours or in conjunction with other sedation prone medications.
Always tell your personal physician about any supplements you're taking, even if they're ‘natural’, like progesterone. That way they can check for potential side effects or interactions with other therapy you are on, or are being considered for using.
If these circumstances apply to you, consider consulting an experienced physician when using ongoing and/or higher dosed progesterone therapy for either PMS or migraine.