FAQ Episode 45: Migraine risk factors and your Immune System
Frequently Asked Questions about Natural Migraine Relief for Women
I reviewed an article this week about how various risk factors stimulate immune reponses that can provoke migraine headaches. It was absolutely fascinating, but technically very deep. At the risk of being simplistic, I’m going to give you a thumbnail sketch of the findings, with one very clear call to action at the conclusion.
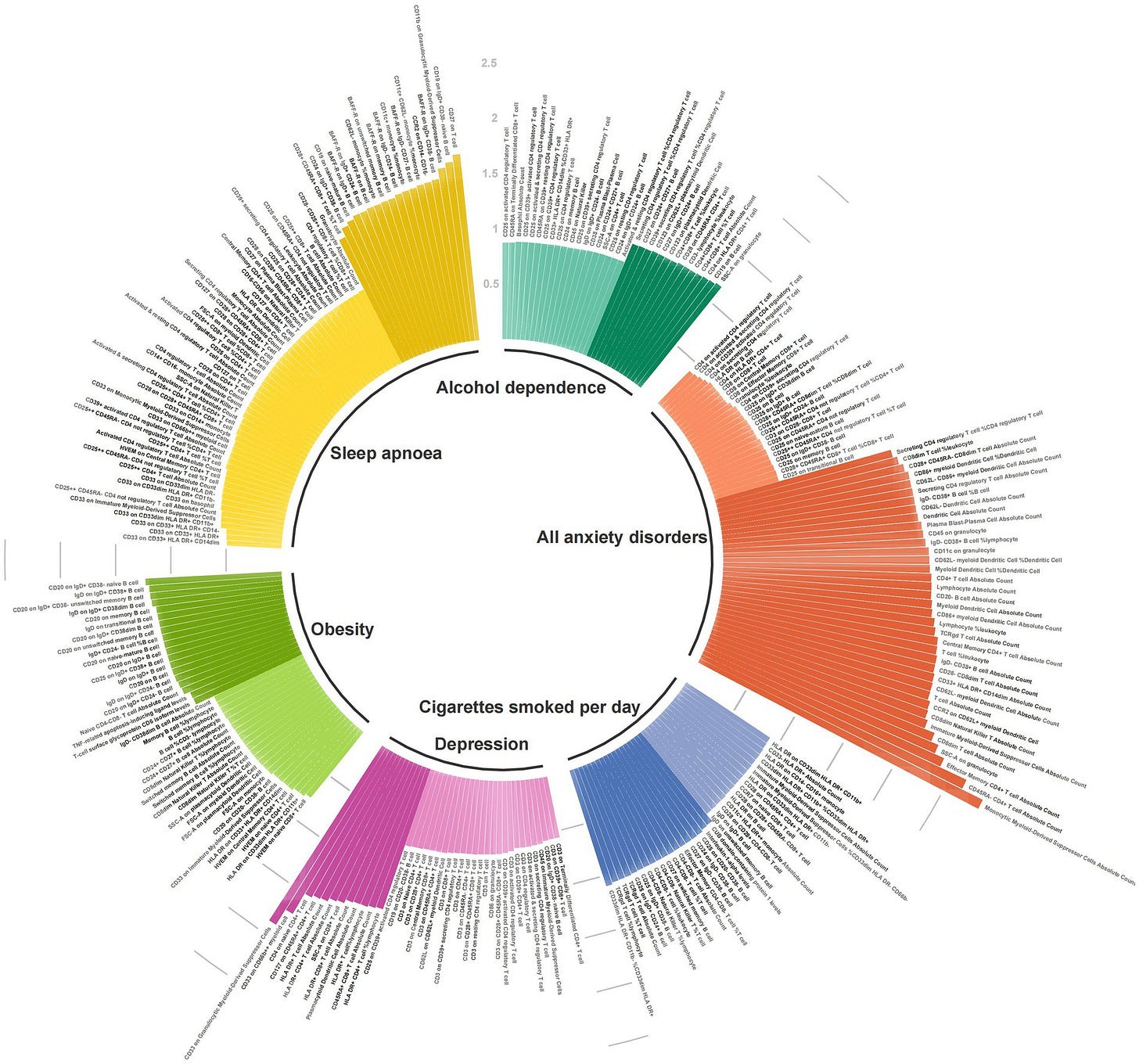
The article was published this last week in the journal Frontiers in Neurology1 and titled “Inflammo-immune perspective on the association of eight migraine risk factors with migraine.” The study looked at multiple studies involving seven migraine risk factors, and looked at levels of 91 circulating inflammatory proteins and 731 immune cells for each of them. Inflamation is probably the leading family of root cause factors that produce migraines, and many other diseases as well. Because of this, I devote two full lessons to this topic in my Natural Migraine Relief course.
Risk factors that this study included were: cigarette smoking, obesity, alcohol dependance, depression, different types of anxiety disorders, insomnia with sleep apnea, and glucocorticoid (steroid) use. The study found that there was a significant risk of migraine association found in 23 immune cells and inflammatory proteins that correlated with the risk factors of:
depression
all anxiety disorders
sleep apnea
and less so for alcohol use, obesity and smoking. I think most of us would think that these last three would have been found to be major offenders. It goes to show that while any seemingly adverse risk factor can have multiple avenues of insult to our health, it isn’t always by the most obvious routes.
The graphic posted above2 gives an excellent visual representation of the number and magnitude of immune stimulated inflammation associated with each of the risk factors noted in the study. Longer lines represent greater degrees of immune mediated inflammation.
Take home points from this article:
Even though these risk factors all look different on paper, through their effect on the immune system they share a common promoting factor for migraines, and that is inflammation. If you remember my “full cup theory of migraine” example (about the fifth paragraph down on this link), its not just one provocative factor, but rather the accumulative collection several such factors that results in the clinical expression of the problem, in this case, a migraine headache.
Currently we have very few medical tools that could fine tune the management for each of the 23 immune cells and inflammatory proteins that were identified with the risk factors listed above. Maybe someday, but if the current “new drug” pipeline for migraine meds is any example, they won’t be inexpensive, side-effect free or here soon.
We do have a tool to downregulate excess immune reactivity and improve migraines, no matter which of the risk factors are at play. It is available now, its inexpensive, very safe when taken in your right dose, and it has proven efficacy for migraine headaches.34 That would be getting to an optimal level of Vitamin D3. One of the studies I cited showed that healthy Vitamin D levels cut migraines more than 50% for more than half of those studied. While more than half of these migraineurs saw benefit, it was not the single item cure all for these individuals. And that is because every migraine has multiple contributory root cause factors that need to be identified and addressed. The more you find and address, the better you will do.
You can find much more about Vitamin D and its proper dosing in my post FAQ Episode 11: Migraine prevention: Make sure you don’t ‘fall back’ on your Vitamin D3 level.
Vitamin D is only one of several nutrients where a deficit can contribute to migraine headaches. My paid subscribers can find much more on this at: Lesson 19: Nutrient deficits as a Root Cause factor in Migraines from my Natural Migraine Relief for Women course.
In a health care world dominated by medical-industrial-complex groupthink, its essential to have a balanced perspective on the role of drug therapy in managing medical problems. As one of my favorite integrative physician colleagues Dr. Robert Rowan puts it: “There is not a single chronic degenerative disease which arises from a deficiency of a synthetic petrochemical pharmaceutical.”
Please remember that finding and addressing the root causes of your migraine or other health disorders is always the best pathway to recovery.
If you want to visit Dr. Rowan’s blog site where he has free blog posts, go to
“Inflammo-immune perspective on the association of eight migraine risk factors with migraine: a multi-omics Mendelian randomization study” Jiaxi Zhao, et. al. Front. Neurol., 06 August 2024 Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1440995
ibid page 2
Cincinnati Children's Hospital Medical Center. "Many with migraines have vitamin deficiencies, says study." ScienceDaily. ScienceDaily, 10 June 2016. <www.sciencedaily.com/releases/2016/06/160610140645.htm>.
Curr Med Res Opin. A randomized, double-blinded, placebo-controlled, parallel trial of vitamin D3 supplementation in adult patients with migraine. Gazerai, P et.al. 2019 Apr;35(4):715-723. doi: 10.1080/03007995.2018.1519503. Epub 2018 Sep 28.